 In the mid-1990s the most highly touted location for the optimal use of telemedicine was in remote areas where there are fewer physicians. The argument was that the absence of specialists could be remedied by “porting in” radiologists and ophthalmologists via a hard wire connection. We realized the need was just as great within inner cities. We used DSL connectivity to set up video psychiatry appointments for underserved kids and moms four miles away at California Hospital just across the LA River.
In the mid-1990s the most highly touted location for the optimal use of telemedicine was in remote areas where there are fewer physicians. The argument was that the absence of specialists could be remedied by “porting in” radiologists and ophthalmologists via a hard wire connection. We realized the need was just as great within inner cities. We used DSL connectivity to set up video psychiatry appointments for underserved kids and moms four miles away at California Hospital just across the LA River.
HCP Principals Stumpf and Zalunardo were recognized as among the first to integrate telemedicine protocols and systems in the medical mainstream. In 1996 the USC Advanced Biotelecommunications and Bioinformatics Center (ABBC) received one of the first federal grants supporting the establishment of telemedicine models in regular analog paper based medical practices. The funding agency was the National Library of Medicine. The project was funded for five years at $1 million each year. Our approach was to use digital imaging as the technological platform to capture and distribute images to radiologists, ophthalmologists, infectious disease physicians, and family physicians. The demonstration was a resounding success. We presented our outcomes report at the National Library of Medicine which had funded our five year multi-site proposal. We showed that telemedicine could indeed enhance – even replace – legacy systems for reviewing and grading images of eyes, skin, x-rays…anything that converted to digital formats. [Ask us for the report.]
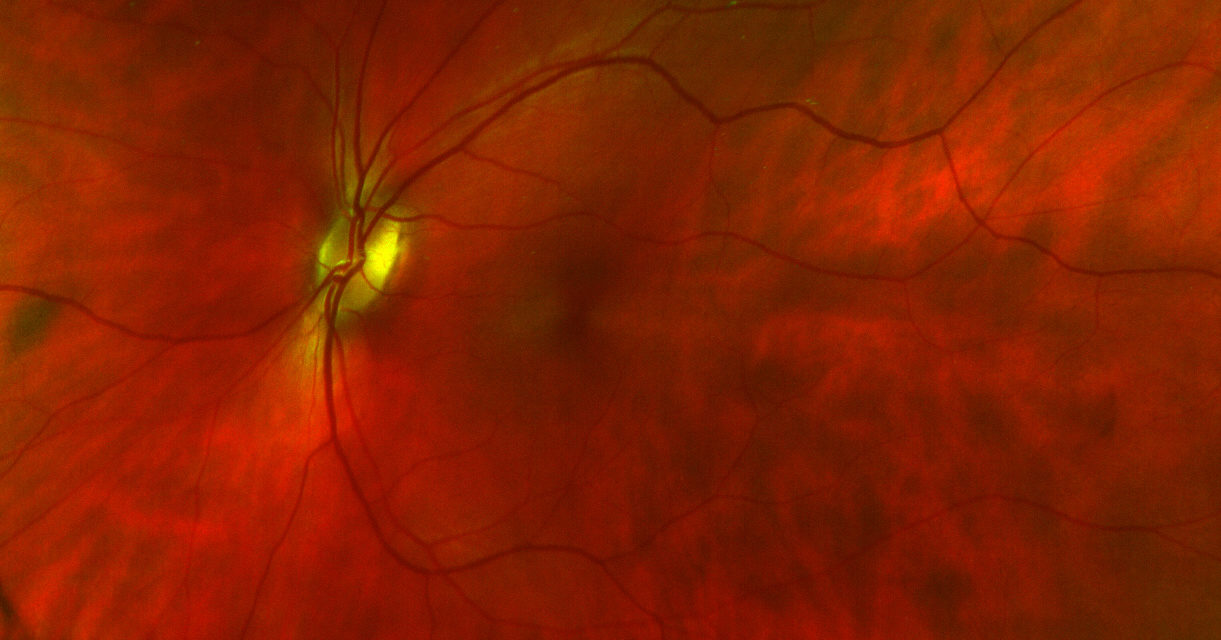
Our telemedicine group – the ABBC – caught the attention of retina imaging companies featuring breakthrough ideas. Optos.com asked us in 2000 to evaluate their novel wide scan retina imaging technology [the featured image for this post].
We persuaded multiple private foundations, e.g., Queens Care, The California Endowmen, to support expansion as the Latino DREaM: Diabetic Retinopathy Evaluation and Management. This project proved that telehealth could improve healthcare access for underserved inner city populations. Today – circa 2019/2020 there is no telemedicine. There is only digital healthcare.
Healthcare IT News published a piece in January 2019 on a Chicago hospital system that aims to be among the first such orgs to deploy 5G [https://www.healthcareitnews.com/news/rush-become-first-5g-hospital-system-us]. Near the end of the brief piece – which is worth reading – is the following paragraph.
“Remote medicine, while hardly a new phenomenon, is growing at leaps and bounds both in terms of the quality of data that can be captured, sent and computed, as well as the speed at which it can be transferred. Greater network speeds mean that the trend of “anytime, anywhere” medicine will continue to grow.”
REMOTE MEDICINE. This is what telemedicine always promised. It just took a couple of decades for the technology to become a practice standard. Of course, today’s tech includes so much more, most often delivered via cell phones. Medicine is moving from control by providers and HMOs to control by users. It is all about the technology…and improving quality and access while decreasing costs.